BLOG

Causes and Relief for Cracked Heels
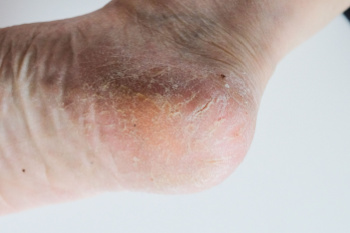
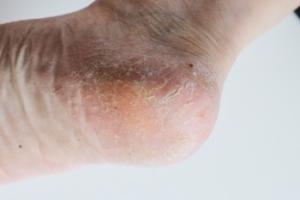
Cracked heels, or heel fissures, are a common foot problem where the skin on the heels becomes dry, thickened, and splits. These cracks can cause discomfort and pain, especially while standing or walking, and they can sometimes lead to infection if left untreated. Heel fissures occur when the skin loses moisture, leading to dryness and reduced elasticity. Contributing factors include prolonged standing, wearing open-backed shoes, obesity, and conditions like diabetes or eczema, which can cause dryness. Relief involves moisturizing the feet regularly with thick emollients or foot creams containing urea or lactic acid to soften the skin. In more severe cases, medical treatment may be necessary, such as debridement or the application of special wound dressings. If you have severely cracked heels, it is suggested that you schedule an appointment with a podiatrist for an examination and treatment.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact one of our podiatrists from Livingston Foot Care Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our office located in North Bellmore, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
How to Know if You Have Gout

Gout is a form of arthritis caused by a buildup of uric acid crystals in the joints, leading to sudden and intense pain. Common symptoms include severe joint pain, typically in the big toe, along with swelling, redness, and warmth in the affected area. The pain often starts at night or early morning and can become excruciating within hours. A gout flare-up usually lasts between three to 10 days, with the most severe symptoms occurring in the first 24 to 48 hours. It may subside on its own but can return if left untreated. To handle a gout flare-up, rest the affected joint, and it is suggested that you contact a podiatrist for an appointment and examination. This type of doctor can prescribe medications such as colchicine or corticosteroids that can help reduce symptoms.
Gout is a painful condition that can be treated. If you are seeking treatment, contact one of our podiatrists from Livingston Foot Care Specialists. Our doctors will treat your foot and ankle needs.
What Is Gout?
Gout is a form of arthritis that is characterized by sudden, severe attacks of pain, redness, and tenderness in the joints. The condition usually affects the joint at the base of the big toe. A gout attack can occur at any random time, such as the middle of the night while you are asleep.
Symptoms
- Intense Joint Pain - Usually around the large joint of your big toe, and it most severe within the first four to twelve hours
- Lingering Discomfort - Joint discomfort may last from a few days to a few weeks
- Inflammation and Redness -Affected joints may become swollen, tender, warm and red
- Limited Range of Motion - May experience a decrease in joint mobility
Risk Factors
- Genetics - If family members have gout, you’re more likely to have it
- Medications - Diuretic medications can raise uric acid levels
- Gender/Age - Gout is more common in men until the age of 60. It is believed that estrogen protects women until that point
- Diet - Eating red meat and shellfish increases your risk
- Alcohol - Having more than two alcoholic drinks per day increases your risk
- Obesity - Obese people are at a higher risk for gout
Prior to visiting your podiatrist to receive treatment for gout, there are a few things you should do beforehand. If you have gout you should write down your symptoms--including when they started and how often you experience them, important medical information you may have, and any questions you may have. Writing down these three things will help your podiatrist in assessing your specific situation so that he or she may provide the best route of treatment for you.
If you have any questions, please feel free to contact our office located in North Bellmore, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Everything You Need to Know About Gout
Gout, typically found in diabetic patients, is an unusually painful form of arthritis caused by elevated levels of uric acid in the bloodstream. The condition typically strikes the big joint on the big toe. It has also been known to strike the knees, elbows, fingers, ankles and wrists—generally anywhere that has a functioning, moving joint.
The high level of uric acid in a person’s bloodstream creates the condition known as hyperuricema—the main cause of gout. Genetic predisposition occurs in nine out of ten sufferers. The children of parents who suffer gout will have a two in ten chance of developing the condition as well.
This form of arthritis, being particularly painful, is the leftover uric acid crystallizing in the blood stream. The crystallized uric acid then travels to the space between joints where they rub, causing friction when the patient moves. Symptoms include: pain, redness, swelling, and inflammation. Additional side effects may include fatigue and fever, although reports of these effects are very rare. Some patients have reported that pain may intensify when the temperature drops, such as when you sleep.
Most cases of gout are easily diagnosed by a podiatrist’s assessment of the various symptoms. Defined tests can also be performed. A blood test to detect elevated levels of uric acid is often used as well as an x-ray to diagnose visible and chronic gout.
Treatment for gout simply means eliminating symptoms. Non-steroid anti-inflammatory drugs or NSAIDs (Colchicine and other corticosteroid drugs, etc.) will quell the redness, the swelling, and the inflammation. However, managing your diet, lifestyle changes, and using preventative drugs are all helpful toward fully combating the most severe cases.
Those that lead an inactive lifestyle are at a higher risk for gout. Any amount of exercise decreases the probability of repeat encounters with the condition. Reducing your consumption of red meat, sea food, and fructose-sweetened drinks also reduces the likelihood of chronic gout as well.
Ingesting Vitamin C, coffee, and particular dairy products can help with maintaining a healthy lifestyle. There are new drugs out on the market that inhibit the body’s production of uric acid-producing enzymes. However, reducing or eliminating your overall levels of uric acid is the best remedy to ensuring you lead a gout-free life.
Wound Care for Diabetic Foot Ulcers

Diabetic foot ulcers are a common complication for people with diabetes. They are caused by issues like peripheral neuropathy, poor circulation, and increased pressure on certain areas of the foot. Neuropathy can reduce sensation in the feet, leading to unnoticed injuries that may worsen or become infected. In addition, reduced blood flow slows the healing process, which further increases the risk of infection. Podiatrists are equipped to assess the severity of diabetic foot ulcers and provide appropriate wound care. This includes removing dead tissue, applying specialized dressings, and offloading pressure from the affected area. In some cases, surgery may be required to support the healing process. Proper care is essential to minimize the risk of serious complications, such as gangrene or amputation. By addressing the specific needs of the foot ulcer, a podiatrist can help promote recovery and reduce further risks. If you have a diabetic foot ulcer, it is suggested that you make an appointment with a podiatrist for wound care options.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with one of our podiatrists from Livingston Foot Care Specialists. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in North Bellmore, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Symptoms and Causes of Ankle Pain

Ankle pain can also result in swelling, and stiffness. While the pain may be sharp, dull, or throbbing, it often intensifies with movement or pressure. Swelling surrounding the ankle can indicate inflammation or injury, leading to visible puffiness and discomfort. Stiffness in the joint can limit mobility, making it difficult to flex or extend the ankle fully. Common causes of ankle pain include sprains, strains, and fractures from trauma or overuse. Conditions like arthritis or tendinitis can also contribute to chronic pain and swelling. A proper diagnosis by a podiatrist is vital to determine the underlying cause and guide appropriate treatment. If you have ankle pain, it is suggested that you contact a podiatrist to determine the cause and offer treatment solutions.
Ankle pain can have many different causes and the pain may potentially be serious. If you have ankle pain, consult with one of our podiatrists from Livingston Foot Care Specialists. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Ankle pain is any condition that causes pain in the ankle. Due to the fact that the ankle consists of tendons, muscles, bones, and ligaments, ankle pain can come from a number of different conditions.
Causes
The most common causes of ankle pain include:
- Types of arthritis (rheumatoid, osteoarthritis, and gout)
- Ankle sprains
- Broken ankles
- Achilles tendinitis
- Achilles tendon rupture
- Stress fractures
- Tarsal tunnel syndrome
- Plantar fasciitis
Symptoms
Symptoms of ankle injury vary based upon the condition. Pain may include general pain and discomfort, swelling, aching, redness, bruising, burning or stabbing sensations, and/or loss of sensation.
Diagnosis
Due to the wide variety of potential causes of ankle pain, podiatrists will utilize a number of different methods to properly diagnose ankle pain. This can include asking for personal and family medical histories and of any recent injuries. Further diagnosis may include sensation tests, a physical examination, and potentially x-rays or other imaging tests.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are rest, ice packs, keeping pressure off the foot, orthotics and braces, medication for inflammation and pain, and surgery.
If you have any questions, please feel free to contact our office located in North Bellmore, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ankle Pain
The ankle joint is the point at which the bones of the leg and foot join. This joint is crucial because it is responsible for the foot’s mobility. Ankle pain is typically the result of inflammation from an injury to bones, joint space, cartilage, ligaments, tendons, or muscles in the area. Commonly associated symptoms with ankle pain are bruising, redness, numbness, stiffness, weakness, and tingling.
The most common causes of ankle pain are sprains and injuries. Ankle sprains are one of the most common musculoskeletal injuries. Sprains occur when the ligaments of the ankle become partially or completely torn due to sudden stretching. Sprains can occur on either the inner or outer sides of the ankle joint. Usually, these injuries occur when the ankle is twisted in an activity by stepping off an uneven surface. More specific causes include rheumatoid arthritis, gout, osteoarthritis, and Achilles tendonitis.
If you are experiencing ankle pain, you should consult with your podiatrist to choose the best method of care. Your doctor will conduct an examination of your ankle to determine the underlying cause of the pain.
Arthritis Can Cause Pain in the Feet and Ankles
Foot Care For the Elderly

Elderly foot care is essential for maintaining mobility and preventing complications as people age. Older adults often face issues, such as reduced circulation, weakened muscles, and diminished sensation. These can lead to problems like bunions, hammertoes, and painful calluses. Additionally, diabetes can worsen foot issues, increasing the risk of ulcers, infections, and falls. Proper foot care includes regular inspection for cuts, sores, or changes in skin color, as well as maintaining good hygiene and nail care. Wearing supportive, well-fitting shoes can help prevent pressure sores and provide stability. Regular foot exercises and maintaining a healthy weight can also alleviate discomfort and enhance mobility. To address foot problems effectively and prevent serious complications, it’s suggested you make an appointment with a podiatrist. Their expertise in elderly foot care ensures a comprehensive approach to keeping your feet healthy and functional.
Proper foot care is something many older adults forget to consider. If you have any concerns about your feet and ankles, contact one of our podiatrists from Livingston Foot Care Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
The Elderly and Their Feet
As we age we start to notice many changes in our body, but the elder population may not notice them right away. Medical conditions may prevent the elderly to take notice of their foot health right away. Poor vision is a lead contributor to not taking action for the elderly.
Common Conditions
- Neuropathy – can reduce feeling in the feet and can hide many life-threatening medical conditions.
- Reduced flexibility – prevents the ability of proper toenail trimming, and foot cleaning. If left untreated, it may lead to further medical issues.
- Foot sores – amongst the older population can be serious before they are discovered. Some of the problematic conditions they may face are:
- Gouging toenails affecting nearby toe
- Shoes that don’t fit properly
- Pressure sores
- Loss of circulation in legs & feet
- Edema & swelling of feet and ankles
Susceptible Infections
Diabetes and poor circulation can cause general loss of sensitivity over the years, turning a simple cut into a serious issue.
If you have any questions please feel free to contact our office located in North Bellmore, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.